Insights
Precision machining has become increasingly dependent on the performance of the CNC machine tool holder, a component often underestimated in its influence on accuracy, surface finish, and tool life. With today’s high-speed spindles, multi-axis machining centers, and micro-tolerance production standards, the interaction between dynamic balance, runout behavior, and clamping mechanics has never been more critical. This article provides a neutral, engineering-focused analysis of these performance factors and introduces several leading global manufacturers contributing to advancements in tool-holding technology.
2026-03-02 17:06:33
Scaffolding plays a critical role in structural access, construction workflows, and worker safety. Procurement teams increasingly rely on international standards such as EN74, BS1139, and OSHA 1926 when selecting vendors and evaluating system quality. This article provides a practical, neutral overview of how buyers can assess compliance and compares several notable ring lock scaffolding suppliers serving global markets.
2026-03-02 16:58:14
In the high-pressure environment of B2B manufacturing, the line between profit and loss is often drawn on the shop floor. Procurement managers and factory owners are constantly bombarded with cost-saving initiatives. Usually, these focus on negotiating raw material prices or reducing energy consumption. However, one of the most significant levers for profitability is often overlooked because it is viewed as a simple consumable: the Tool Holder.
2026-02-25 11:28:04
As manufacturers pursue energy efficiency and carbon reduction, hydraulic systems are being re-engineered to meet green manufacturing standards. Modern Hydraulic Power Units (HPUs), enabled by servo pumps and intelligent control, now deliver on-demand power with significantly lower energy loss, noise, and heat generation.
2026-02-25 11:17:33
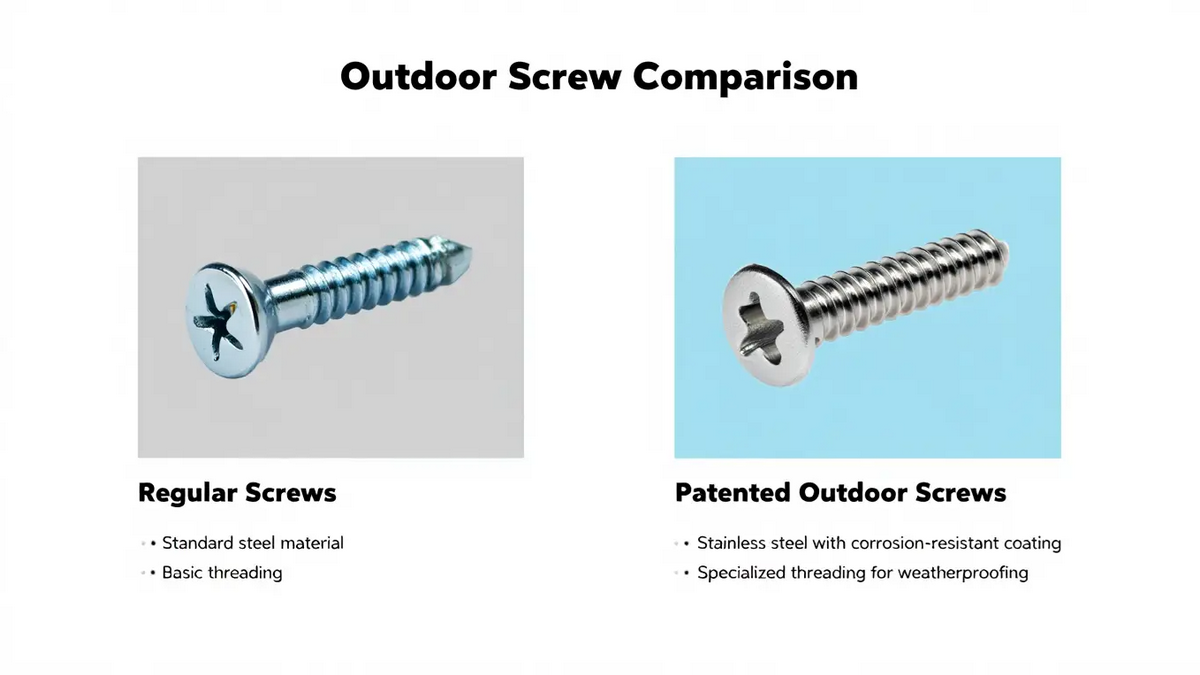
In today’s construction industry, the durability of exterior walls and roof assemblies depends not only on design or materials but also on the Patent Screws that secure them. These fasteners endure constant exposure to moisture, UV light, and temperature changes. Traditional screws often fail under these conditions, causing corrosion, leaks, or costly maintenance. This article explores how Patent Screws, with their patented coatings and sealing systems, help engineers and procurement professionals achieve long-term reliability in demanding environments.
2026-02-11 08:53:24
In the manufacturing sector, integrated workflows for plastic production—from recycling to film extrusion, bag making, and printing—play a crucial role in enhancing efficiency and sustainability. These systems enable manufacturers to handle the full lifecycle of plastic materials, addressing environmental concerns while optimizing operational costs. As industries shift toward circular economies, understanding these processes provides valuable insights for both new entrants and established operations seeking upgrades.
2026-02-11 08:44:50
As industrial automation, precision machining, and sustainability reshape global manufacturing, procurement managers face mounting pressure to balance cost, reliability, and innovation. Hydraulic systems remain essential to industries ranging from machine tools and plastics to metal forming and robotics — and the hydraulic pump sits at the core of every efficient system.
2026-02-03 09:31:17
The global demand for bubble tea is driving stricter requirements for ingredient sourcing, making food certifications and Halal standards essential for market access. Suppliers of tapioca pearls, flavored syrups, and toppings must comply with recognized food-safety frameworks like ISO 22000 and FSSC 22000, while Halal certification ensures products meet Islamic dietary laws for Muslim-majority markets. Together, these certifications not only safeguard quality and safety but also enable manufacturers, café owners, and distributors to expand their reach with confidence when sourcing OEM/ODM bubble tea ingredients and other bubble tea supplies.
2026-02-03 09:15:06
As the event and stage engineering industry faces increasing demands for speed, safety, and sustainability, temporary structures must evolve beyond traditional construction methods. Modular scaffolding has become a core infrastructure solution, redefining how large-scale events are built, managed, and optimized.
2026-01-27 16:27:32
In industrial packaging—particularly for chemicals, paints, and coatings—three-piece metal cans must endure extreme conditions: aggressive chemical formulations, internal pressurization, and long-term storage stability. Unlike beverage or food-grade containers, these applications demand superior corrosion resistance, leak-proof sealing, and structural robustness. Meeting these requirements starts not with the can itself, but with the can-making equipment that produces it. Manufacturers like Shin-I Machinery Works Co., Ltd. are rising to this challenge, offering specialized machinery designed explicitly for non-food, high-performance packaging. This article explores the critical design and production considerations for industrial three-piece cans, outlines key equipment selection criteria, and highlights leading global suppliers—including Shin-I—serving this demanding sector.
2026-01-27 16:09:29
Hot Topic
Agree





.jpg)



