The global number of premature births is increasing annually, with immature lungs being the primary cause of neonatal respiratory distress syndrome (RDS). In the United States alone, approximately 40,000 infants are affected yearly, and some survivors may suffer chronic respiratory complications. The incidence of RDS exceeds 80% in infants born before 28 weeks gestation. Traditional high-frequency or mechanical ventilation can improve oxygenation but carries risks such as airway injury from intubation, chronic lung disease, and prolonged hospitalization, alongside high consumable and staffing costs.
Emerging Trend: Non-Invasive Support
Due to the risks associated with endotracheal intubation—including airway trauma, chronic lung disease, and extended hospital stays—and its heavy demand on medical resources and personnel, neonatal RDS care is shifting toward a lung-protective ventilation strategy. This approach aims to minimize lung injury and improve survival rates through appropriate oxygenation, non-invasive respiratory support, and early administration of exogenous surfactants. This care model is especially suitable for infants weighing less than 1500 grams and extremely preterm neonates.
Bubble CPAP (Continuous Positive Airway Pressure) is widely regarded as the reliable and low-risk first-line non-invasive respiratory support method for treating neonatal RDS. It works by submerging the expiratory limb of the breathing circuit into a water column to generate stable airway pressure. Without requiring complex motors or digital controls, its simplicity, reliability, and cost-effectiveness have led to widespread adoption in low-resource healthcare settings globally (Wikipedia).
Clinical studies show that compared to traditional ventilator CPAP (V-CPAP), Bubble CPAP yields lower complication rates, shorter hospital stays, and overall cost-effectiveness, providing higher value to healthcare systems and families alike.
Integrated, User-Oriented Kit Design
Lightweight, Flexible Nasal Prongs (nCPAP Prong)
Made of soft silicone with a matte flat finish, available in sizes #0 to #7, these prongs fit various infant nostrils while minimizing skin pressure and injury.
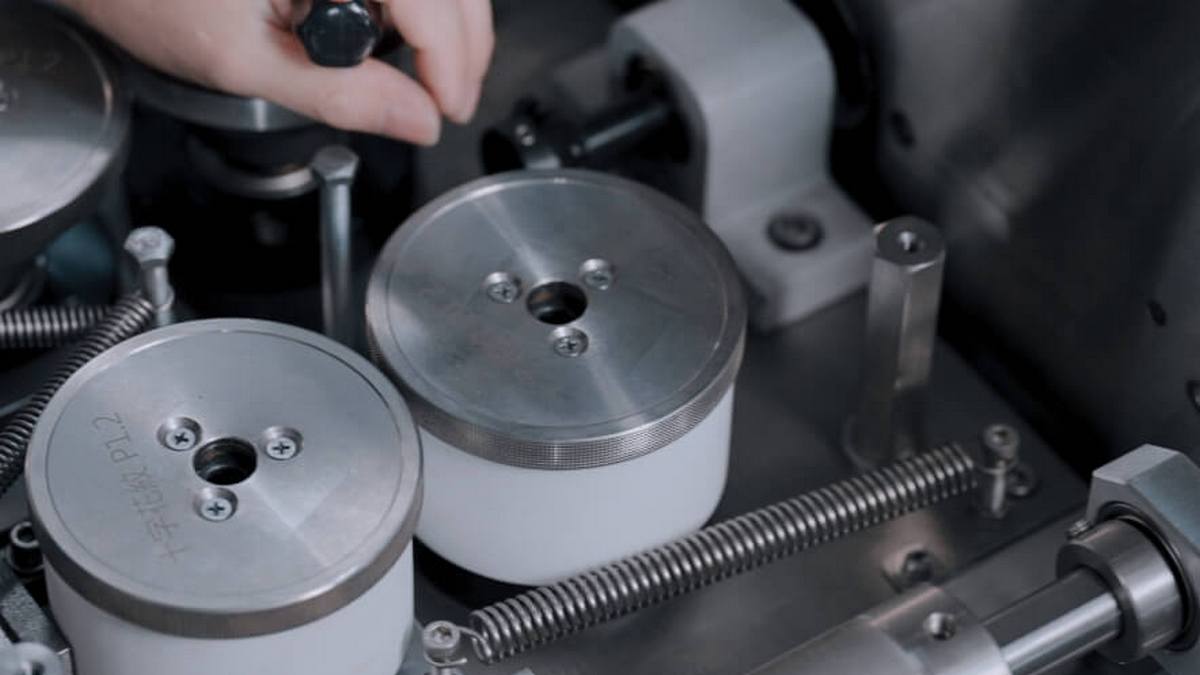
Safe and Stable Breathing Circuit Assembly
Standard bubble PAP valves allow precise pressure adjustment from 0 to 10 cmH₂O via an easy-turn lever.
Pressure monitoring catheters enable real-time, transparent pressure feedback when connected to monitoring devices.
Flexible 20 cm tubing with color-coded inspiratory and expiratory limbs ensures easy placement, identification, and reduces displacement risks.
Secure Headgear (nBonnet)
Features an open-band design with cotton and Velcro straps to minimize nasal prong slippage and improve interface stability, compatible with various head shapes.
Connector and Interface Compatibility
Interfaces are highly compatible with diverse respiratory system tubing, facilitating integration with humidifiers, exhaust gas collection modules, and oxygen delivery devices—adapted to the complex needs of NICU environments.
External Trends and Industry Outlook
Approximately 15 million premature infants are born worldwide annually, with a large proportion concentrated in emerging markets such as Southeast Asia and South Asia. Due to relatively limited healthcare resources, Bubble CPAP’s low cost, ease of use, and stable airway pressure maintenance have made it the preferred respiratory support method in neonatal and pediatric hospitals within these regions.
Meanwhile, environmental and cost pressures drive increasing adoption of high sterilization-tolerant silicone components, extending device lifecycles and supporting ESG management compliance.
With the rise of home care and telemedicine services, these durable and easy-to-clean integrated respiratory support kits meet the growing demands for post-discharge hypoxia follow-up and remote monitoring.
Conclusion
When premature infants face severe respiratory risks, a lightweight respiratory support kit equipped with Bubble CPAP can provide stable, narrow-range positive pressure, minimizing the risks associated with invasive ventilation. Beyond immediate clinical benefits, its high reliability, operability, and reusability align seamlessly with global healthcare trends, positioning it as the emerging international standard for neonatal respiratory support technology.
From the moment the first bubble rises along the edge of the alveolus, it symbolizes the newborn’s second call to life. The proliferation of such devices marks an industry evolution from “aggressive intubation” to “gentle support,” enhancing treatment quality and carrying the hope for every infant’s sustained breath.










.jpg)


